The Ferritin Test Doctors Don't Order: Why Low Iron Storage Is Sabotaging Your Mental Health
December 4, 2025
You're exhausted. You've told your doctor multiple times. They ran labs. Everything came back "normal." But you don't feel normal—you feel terrible. And you're starting to wonder if it's all in your head.
It's not. Let me show you what they missed.
---
Marcus was 28, working 60-hour weeks at a tech startup in downtown LA. He'd been to three different doctors in the past year, complaining of crushing fatigue, brain fog that made simple coding tasks feel impossible, and depression that wouldn't lift despite two different antidepressants. Every time, he heard the same thing: "Your labs look normal."
His CBC was perfect. Hemoglobin: 15.2 g/dL. No anemia. His thyroid was fine. His metabolic panel showed healthy kidney and liver function. On paper, Marcus was the picture of health.
But he felt terrible.
What none of those doctors checked was his ferritin level. When I finally ordered it, the number came back at 18 ng/mL—technically within the "normal range" of 12-300 ng/mL, but nowhere near the 75-100 ng/mL that the brain needs to produce neurotransmitters efficiently.
Within three months of iron supplementation, Marcus's ferritin climbed to 82 ng/mL. His energy returned. The brain fog lifted. And his depression—the symptom that had sent him seeking psychiatric care—improved by 60% without changing his antidepressant.
This isn't a miracle story. It's diagnostic medicine applied to psychiatry.
I practice diagnostic psychiatry in Los Angeles and Phoenix, with telehealth available throughout California and Arizona.
What Is Ferritin and Why Your Brain Desperately Needs It
After 19 years in ICU nursing across seven specialties at top-tier hospitals including Cedars-Sinai and USC Keck, I learned one fundamental truth: when patients are critically ill, you don't guess—you systematically investigate every possible cause. I apply that same diagnostic rigor to psychiatric symptoms, because the body always tells a story. Psychiatric symptoms are often the final chapter of an untold medical narrative.
Ferritin is your body's iron storage protein. Think of it as your iron savings account. When your body needs iron to build red blood cells, produce energy, or manufacture neurotransmitters, it withdraws iron from your ferritin reserves.
Here's what most people don't understand: your body will sacrifice your brain function to keep your blood oxygenated.
Iron is essential for three critical brain functions:
1. Neurotransmitter Production
Iron is required for tyrosine hydroxylase—the enzyme that converts tyrosine into dopamine
Iron is required for tryptophan hydroxylase—the enzyme that converts tryptophan into serotonin
Without adequate iron, your brain literally cannot manufacture the chemicals that regulate mood, motivation, and energy
2. Myelination
Iron is necessary for myelin production—the insulation around nerve fibers that allows rapid signal transmission
Low iron = slower brain processing = brain fog and cognitive dysfunction
3. Mitochondrial Function
Iron-containing enzymes are critical for cellular energy production
Low iron stores = less cellular energy = crushing fatigue that no amount of caffeine can touch
The Ferritin vs. Hemoglobin Confusion: Why Your "Normal" CBC Means Nothing
Here's the critical mistake most doctors make: they check a CBC (Complete Blood Count) and see normal hemoglobin, so they conclude iron isn't the problem.
This is fundamentally flawed reasoning.
Your body has a hierarchy of iron needs:
1. First priority: Keep red blood cells functioning (hemoglobin production)
2. Second priority: Everything else—including your brain
When iron stores begin to deplete, your body pulls from ferritin reserves to maintain hemoglobin production. Your CBC stays normal for months or even years while your ferritin plummets. This condition is called Iron Deficiency Without Anemia (IDWA)—and it's twice as common as iron deficiency anemia.
Let me break down the timeline:
Stage 1: Depleted Iron Stores (Ferritin <30 ng/mL)
CBC: Normal
Hemoglobin: Normal
Symptoms: Fatigue, brain fog, low mood, restless legs
What doctors typically say: "Your labs are fine"
Stage 2: Iron Deficiency Without Anemia (Ferritin <15 ng/mL)
CBC: Normal or borderline
Hemoglobin: Still normal (barely)
Symptoms: Severe fatigue, depression, anxiety, cognitive impairment, hair loss, brittle nails
What doctors typically say: "Maybe you're just stressed"
Stage 3: Iron Deficiency Anemia (Ferritin <10 ng/mL)
CBC: Abnormal (low hemoglobin, microcytic anemia)
Hemoglobin: Low
Symptoms: Everything above PLUS shortness of breath, dizziness, pale skin
What doctors finally say: "You're anemic. Let's treat this."
Most patients I see are stuck in Stage 1 or 2. Their ferritin is 15-40 ng/mL—low enough to cause severe psychiatric symptoms, but high enough that their CBC looks "normal" and their primary care doctor tells them nothing is wrong.
Research indicates that iron deficiency is significantly more common in patients with depression than in the general population. Multiple studies have found prevalence rates ranging from 40-80% depending on the population studied, yet standard psychiatric evaluations rarely check ferritin levels. This is a massive blind spot in mental health care.
Why Don't Doctors Order the Ferritin Test?
If ferritin is so important, why isn't it routinely checked? Four reasons:
1. It's Not in Standard Panels
When your doctor orders "routine labs," they're checking CBC, metabolic panel, maybe thyroid. Ferritin isn't included. It has to be specifically added, and if the doctor isn't thinking about iron storage, they won't order it.
2. Medical Training Focuses on Anemia
Physicians are trained to identify and treat iron deficiency anemia—the condition where hemoglobin drops and patients become symptomatic with shortness of breath and dizziness. IDWA (Iron Deficiency Without Anemia) isn't emphasized in medical education, despite being twice as common.
3. Insurance and Cost Barriers
Some insurance plans question ferritin testing if the CBC is normal. Doctors avoid tests that might get denied or require prior authorization. It's easier to skip the ferritin and focus on what's "obviously" needed.
4. Lack of Awareness About Psychiatric Connection
Most doctors don't connect low ferritin with depression, anxiety, and brain fog. If you come in complaining of mental health symptoms, they're thinking antidepressants—not iron studies.
This creates a perfect storm: patients suffering from correctable iron deficiency are told their labs are "normal" and sent home with prescriptions for medications they may not need.
Normal Range vs. Optimal Range: The Lab Result Lie
Here's where the medical system fails patients systematically.
The "normal" ferritin range on standard lab reports is typically 12-150 ng/mL for women and 12-300 ng/mL for men.
This range is designed to identify severe iron deficiency (anemia), not optimal brain function.
Based on extensive research into ferritin and psychiatric symptoms, here's what the ranges actually mean:
| Ferritin Level | Lab Interpretation | Reality for Brain Function |
|----------------|-------------------|----------------------------|
| <15 ng/mL | Deficient | Severe psychiatric symptoms likely |
| 15-30 ng/mL | "Normal" | Inadequate for neurotransmitter production |
| 30-50 ng/mL | "Normal" | Suboptimal; fatigue and mood issues common |
| 50-75 ng/mL | "Normal" | Borderline adequate |
| 75-100 ng/mL | "Normal" | Optimal for symptom resolution |
| 100-200 ng/mL | "Normal" | Adequate, possibly excellent |
| >300 ng/mL | High | May indicate inflammation or hemochromatosis |
When I review labs with patients, I explain it this way: "Your ferritin is 22. The lab says that's 'normal' because it's above 12. But 12 is the cutoff to prevent anemia—not the level needed for your brain to make dopamine and serotonin efficiently. We need to get you to 75-100."
Studies support this approach:
Research in Neuropsychobiology found that ferritin levels below 50 ng/mL were associated with significantly higher rates of depression and fatigue
A study in Journal of Psychopharmacology showed that patients with treatment-resistant depression had significantly lower ferritin levels than healthy controls
Multiple studies on Restless Legs Syndrome (RLS)—which causes severe sleep disruption and secondary psychiatric symptoms—show that symptoms don't resolve until ferritin reaches 75-100 ng/mL, even if it's "technically normal" at 30-40 ng/mL
Your brain doesn't care what the lab's reference range says. It needs iron to function.
Psychiatric Symptoms of Low Ferritin: More Than Just Tiredness
When patients come to my practice, I'm investigating all possible causes—not just accepting that symptoms are "purely psychiatric." Low ferritin creates a constellation of symptoms that look exactly like primary psychiatric illness:
Depression
Persistent low mood and anhedonia (inability to experience pleasure)
Loss of motivation and interest
Negative thought patterns
Why: Insufficient dopamine and serotonin production due to low iron cofactors
Anxiety
Generalized worry and rumination
Difficulty calming down
Panic symptoms
Why: Neurotransmitter imbalance affects emotional regulation circuits
Brain Fog and Cognitive Dysfunction
Difficulty concentrating or focusing
Slower processing speed
Memory problems
Word-finding difficulties
Why: Impaired myelination and reduced mitochondrial energy production
Crushing Fatigue
Tired despite 8+ hours of sleep
Fatigue that worsens with physical activity (post-exertional malaise)
Need for frequent naps
Why: Mitochondrial dysfunction and cellular energy deficit
Mood Instability and Irritability
Quick to anger or frustration
Emotional volatility
Decreased stress tolerance
Why: Neurotransmitter dysregulation and reduced brain energy reserves
Restless Legs Syndrome (RLS)
Uncomfortable sensations in legs, especially at night
Irresistible urge to move legs
Sleep disruption leading to daytime exhaustion
Why: Low iron in brain regions controlling movement
Unusual Cravings
Ice chewing (pagophagia)—a specific marker of iron deficiency
Craving non-food items (pica)
Why: Unclear mechanism, but strongly associated with low iron
If you're experiencing multiple symptoms from this list, ferritin should absolutely be checked—regardless of what your CBC shows.
Who Needs Ferritin Testing? High-Risk Groups
Certain populations are at significantly higher risk for iron deficiency without anemia:
1. Women with Heavy Menstrual Periods
Monthly blood loss depletes iron stores faster than diet can replace them. Women lose approximately 1 mg of iron per day through menstruation. If your periods are heavy (soaking through pads/tampons frequently, clots, periods lasting >7 days), you're losing even more.
2. Vegetarians and Vegans
Plant-based iron (non-heme iron) is absorbed at only 2-20% efficiency, compared to 15-35% for heme iron from meat. Even with iron-rich plant foods, vegetarians often can't maintain optimal ferritin levels without supplementation.
3. Athletes and Regular Exercisers
Exercise increases iron needs through several mechanisms:
Increased red blood cell turnover
Iron loss through sweat
Foot-strike hemolysis (breakdown of red blood cells from impact)
Gastrointestinal microbleeding during endurance exercise
4. Post-Surgical Patients
Any surgery involves blood loss. Even "minor" procedures can deplete iron stores, especially if blood loss wasn't severe enough to cause anemia but significant enough to lower ferritin.
5. People with Gastrointestinal Issues
Celiac disease and inflammatory bowel disease impair iron absorption
Chronic use of proton pump inhibitors (PPIs) for acid reflux reduces stomach acid needed for iron absorption
H. pylori infection can cause chronic low-grade bleeding
6. Frequent Blood Donors
Each blood donation removes approximately 200-250 mg of iron. Frequent donors (every 8-12 weeks) often cannot restore iron stores between donations.
7. Anyone with Treatment-Resistant Psychiatric Symptoms
If you've tried multiple antidepressants without significant improvement, ferritin must be investigated. Research shows that up to 40% of treatment-resistant depression cases have underlying medical factors—and low ferritin is one of the most common.
How to Advocate for Ferritin Testing
You shouldn't need to beg your doctor to order a simple blood test, but the reality is that many won't order ferritin unless you specifically request it. Here's how to advocate effectively:
What to Say to Your Doctor:
"I'd like to have my ferritin level checked. I understand my CBC is normal, but I've read that ferritin can be low even when hemoglobin is normal, and low iron stores can cause fatigue, depression, and brain fog. Can we add ferritin, along with a complete iron panel, to my labs?"
If Your Doctor Resists:
Some doctors will push back, saying "Your CBC is normal, so iron isn't the problem." Here's how to respond:
"I understand that my CBC is normal, which means I don't have anemia. But I've learned that iron deficiency without anemia is common and can cause the exact symptoms I'm experiencing. Research shows that ferritin levels below 50 can affect brain function even when hemoglobin is normal. I'd really like to rule this out as a contributing factor."
What to Request:
Don't just ask for ferritin—ask for a complete iron panel:
Ferritin (iron storage)
Serum iron (circulating iron)
TIBC (Total Iron Binding Capacity)
Transferrin saturation %
This full panel gives a complete picture of your iron status and can identify patterns that ferritin alone might miss.
How to Interpret Your Results:
When you get your results, don't just accept "normal" as reassuring. Ask for the actual number:
"What is my ferritin level specifically?"
"I see it's 28. Can we discuss whether that's optimal for brain function, not just adequate to prevent anemia?"
When to Seek a Second Opinion:
If your doctor:
Refuses to order ferritin despite your request and symptoms
Orders ferritin, finds it's 20-40 ng/mL, and says "it's fine because it's in the normal range"
Dismisses your symptoms as "just stress" or "just depression" without investigating medical causes
...it may be time to see someone who practices diagnostic psychiatry or integrative medicine. You deserve a provider who investigates systematically, not one who relies on incomplete lab panels and dismisses your concerns.
---
Ready for Answers Instead of Guesswork?
If you're tired of being told "your labs are normal" while feeling terrible, I can help. At Horizon Peak Health, I apply 19 years of ICU diagnostic experience to psychiatric care—starting with comprehensive medical investigation before attributing symptoms to psychiatric illness alone.
During your initial 90-minute assessment, we'll:
Review your complete symptom history and medical timeline
Order comprehensive lab panels including ferritin, thyroid, vitamins, hormones, and inflammation markers
Investigate all possible medical causes systematically
Create an evidence-based treatment plan addressing root causes
Most patients see significant improvement within 2-3 months once we identify and treat all contributing factors.
Investment: Initial evaluation and follow-ups covered by most insurance plans (cash rates: $350-450 initial, $150-200 follow-ups; sliding scale available for uninsured). Lab work typically $20 copay with insurance. Most patients achieve stability within 3-6 months and transition to maintenance visits 2-4 times per year.
Serving Psychiatric evaluation in Rancho Palos Verdes, Psychiatric evaluation in Phoenix, Psychiatric evaluation in Chandler, and telehealth throughout California and Arizona.
---
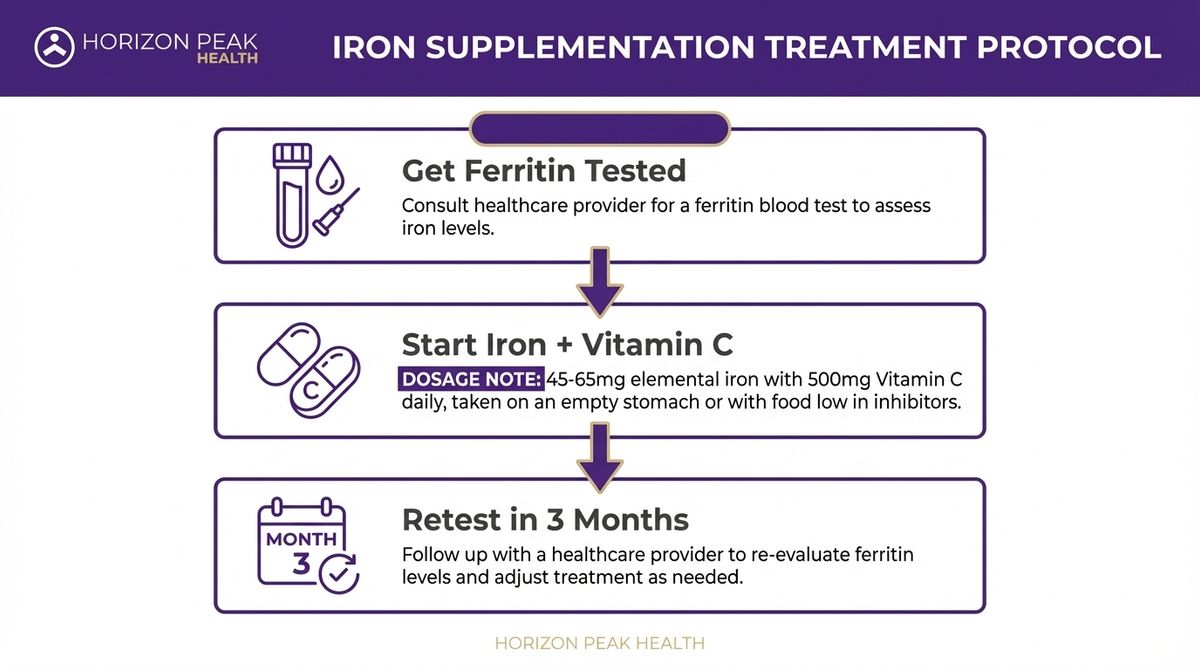
Treatment: Iron Supplementation Done Right
Once low ferritin is identified, treatment is straightforward—but there's a right way and wrong way to do it.
Oral Iron Supplementation
First-Line Treatment:
Ferrous sulfate 325 mg (contains 65 mg elemental iron) once daily
OR Ferrous bisglycinate 25-50 mg (gentler on stomach, better tolerated)
OR Iron polysaccharide complex (for those with GI sensitivity)
How to Take It:
On an empty stomach for maximum absorption (1 hour before meals or 2 hours after)
With vitamin C (orange juice, vitamin C tablet) to enhance absorption
Avoid taking with: Calcium, coffee, tea, or antacids—these block absorption
If GI upset occurs: Take with a small amount of food; absorption decreases but tolerance improves
Expected Timeline:
Symptoms may begin improving in 2-4 weeks
Ferritin increases approximately 10-20 ng/mL per month with consistent supplementation
Target: Reach 75-100 ng/mL for symptom resolution
Full repletion typically takes 3-6 months
Side Effects and Management:
Constipation: Most common side effect; increase water and fiber, consider magnesium supplement
Nausea: Take with small amount of food or switch to gentler form (bisglycinate)
Dark stools: Expected and harmless
Stomach cramping: Usually resolves in 1-2 weeks; if persistent, try lower dose or alternate-day dosing
Monitoring:
Recheck ferritin every 8-12 weeks
Once optimal level reached (75-100 ng/mL), continue supplementation for 3 more months to consolidate stores
Then reassess: some people can stop, others need ongoing maintenance
When IV Iron Is Needed
Oral supplementation works for most people, but some situations require intravenous (IV) iron infusion:
Indications for IV Iron:
Severe iron deficiency (ferritin <10 ng/mL)
Intolerable side effects from oral iron
Gastrointestinal conditions that impair absorption (IBD, celiac, post-bariatric surgery)
Failure to respond to oral iron after 3 months of consistent use
Need for rapid repletion (active bleeding, perioperative period)
IV Iron Protocol:
Iron sucrose (Venofer) or ferric carboxymaltose (Injectafer): 1-2 infusions
Administered in infusion center over 15-60 minutes
Ferritin can increase 100+ ng/mL after a single infusion
Symptoms often improve within 1-2 weeks
Dramatically faster than oral supplementation
Safety:
IV iron is generally well-tolerated. Serious allergic reactions are rare (< 0.1%). Minor side effects include flushing, headache, or muscle aches.
Maintenance After Repletion
Once your ferritin reaches optimal levels, the question becomes: do you need ongoing supplementation?
Who Needs Maintenance:
Women with ongoing heavy periods
Vegetarians/vegans
Athletes
People with absorption issues
Maintenance Dosing:
Ferrous sulfate 325 mg 2-3 times per week (not daily)
OR Continue lower-dose iron (25-50 mg elemental iron) daily
Recheck ferritin every 6-12 months to ensure levels stay optimal
Who Can Stop Supplementation:
Men with correctable cause (post-surgical, temporary increased demand)
Women after menopause
Anyone whose ferritin stays >75 ng/mL for 6+ months without supplementation
Work with your provider to determine your maintenance needs based on individual factors.
The ICU Insight: When High Ferritin Lies
Here's where my ICU training becomes critical. Sometimes ferritin is falsely elevated despite functional iron deficiency—and this can confuse even experienced clinicians.
Ferritin as an Inflammatory Marker
Ferritin is an acute phase reactant, meaning it increases during inflammation, infection, or chronic disease—regardless of actual iron stores. This creates a diagnostic trap:
The Scenario:
Patient has chronic inflammation (autoimmune disease, obesity, chronic infection)
Ferritin level: 150 ng/mL ("normal" or even "high")
Patient assumes iron is fine
But: Iron is actually sequestered in storage and unavailable for use
Symptoms: Fatigue, depression, brain fog—despite "normal" or "elevated" ferritin
This is called anemia of chronic disease or functional iron deficiency.
How to Identify Functional Iron Deficiency
When ferritin is >100 ng/mL but symptoms suggest iron deficiency, order a complete iron panel:
Key Pattern:
Ferritin: Elevated (>100 ng/mL)
Serum iron: Low
TIBC: Low (unlike classic iron deficiency where it's high)
Transferrin saturation: Low (<20%)
PLUS: Elevated CRP (C-reactive protein) or ESR (sedimentation rate)
This pattern shows that iron is locked away in storage (high ferritin) but not available for the body to use (low serum iron, low transferrin saturation). Inflammation drives iron sequestration as a protective mechanism—but it leaves your brain without the iron it needs.
When to Check Inflammation Markers
I routinely check CRP (C-reactive protein) alongside ferritin in patients with:
Autoimmune conditions
Obesity (adipose tissue produces inflammatory cytokines)
Chronic infections
Inflammatory bowel disease
Rheumatoid arthritis or other rheumatologic conditions
If CRP is elevated (>3.0 mg/L) and ferritin is high but transferrin saturation is low, the primary issue is inflammation—not just iron. Treatment involves addressing the underlying inflammatory condition while potentially supplementing iron.
This is advanced diagnostic reasoning that most 15-minute psychiatry appointments don't allow time for. It's why comprehensive assessment matters.
Patient Case Study: From Exhausted to Energized
Let me walk you through a real case that demonstrates everything we've discussed.
Patient: 28-year-old male software engineer, working in downtown LA tech scene
Presenting Complaint:
"I'm exhausted all the time. I can't focus at work. I'm irritable and anxious. My doctor put me on Lexapro two months ago, but I don't feel any better. I sleep 8 hours a night but wake up tired. Coffee doesn't help. I used to love coding, but now even simple tasks feel overwhelming."
Previous Medical Workup (from PCP):
CBC: Normal (Hemoglobin 15.2 g/dL, MCV 88 fL)
Thyroid: Normal (TSH 1.8 mIU/L)
Metabolic panel: Normal
Diagnosis: "Generalized anxiety disorder and depression"
Treatment: Escitalopram 10 mg daily × 2 months (minimal benefit)
My Assessment:
During the 90-minute comprehensive assessment, several key findings emerged:
Symptoms suggesting iron deficiency:
Fatigue worsening with exercise (couldn't finish his usual gym workouts)
Brain fog and slowed processing (work productivity dropped 50%)
Restless legs at night (described as "creepy-crawly feeling" in calves)
Craving ice (chewing ice throughout the day—classic pagophagia)
Risk factors:
Recent half-marathon training (6 months prior)
Vegetarian diet for past 2 years
History of frequent blood donation (donated every 8 weeks until 6 months ago)
Physical exam:
Pale conjunctiva (inside lower eyelids)
Tachycardia (resting heart rate 92 bpm—elevated for his baseline)
Otherwise unremarkable
Labs Ordered:
Ferritin: 18 ng/mL (reference range 12-300 ng/mL)
Iron: 45 mcg/dL (low)
TIBC: 425 mcg/dL (elevated)
Transferrin saturation: 11% (low—normal is 20-50%)
Vitamin D: 28 ng/mL (insufficient)
Vitamin B12: 380 pg/mL (borderline low)
Diagnosis:
1. Major Depressive Disorder with anxious distress—multifactorial
2. Iron deficiency without anemia (ferritin 18 ng/mL)
3. Vitamin D insufficiency
4. Vitamin B12 borderline low
Treatment Plan:
Iron Repletion:
Ferrous sulfate 325 mg daily on empty stomach with orange juice
Target: Ferritin >75 ng/mL
Nutritional Optimization:
Vitamin D3 5,000 IU daily (target 50-70 ng/mL)
Vitamin B12 1,000 mcg sublingual daily (target >600 pg/mL)
Psychiatric:
Continue escitalopram 10 mg daily (don't change during medical optimization)
Reassess need for medication once ferritin and vitamins optimized
Follow-Up Plan:
Recheck labs in 8 weeks
Monthly 30-minute follow-ups to monitor symptoms and adjust treatment
Timeline and Results
Week 2:
Patient reported slight improvement in energy, but still symptomatic. Side effects from iron: mild constipation (managed with increased water and magnesium supplement).
Week 6:
"I'm starting to feel different. The fog is lifting a little. I can focus for longer periods. Still tired, but it's not the crushing exhaustion I had before."
Week 8 (Lab Recheck):
Ferritin: 58 ng/mL (up from 18—good progress)
Vitamin D: 52 ng/mL (optimized)
B12: 680 pg/mL (optimized)
Treatment: Continue iron supplementation to reach target of 75-100 ng/mL.
Week 12:
"I feel like myself again. My energy is back. I'm working out again. The anxiety is 70% better. I can code for hours without my brain shutting down. Even my mood is stable—I'm enjoying things again."
Week 16 (Lab Recheck):
Ferritin: 82 ng/mL (OPTIMAL—target reached)
Treatment: Continue iron 325 mg three times per week for maintenance. Begin tapering escitalopram to assess if still needed.
Week 24 (6 Months Post-Initial Visit):
Ferritin: 88 ng/mL (stable)
Patient off escitalopram entirely
Symptoms: Fully resolved
Plan: Continue maintenance iron supplementation given vegetarian diet and exercise routine. Follow-up every 3 months.
Key Lessons from This Case
1. "Normal" CBC does not rule out iron deficiency. Marcus's hemoglobin was 15.2 g/dL—perfectly normal. But his ferritin was 18 ng/mL—far too low for optimal brain function.
2. Ferritin testing must be specifically ordered. None of his previous doctors checked ferritin because it's not included in routine panels.
3. Symptoms improved progressively as ferritin increased. This wasn't a placebo effect—it was dose-dependent restoration of iron-dependent neurotransmitter synthesis.
4. Multiple nutritional deficiencies often coexist. Marcus also had insufficient vitamin D and borderline B12, both of which contributed to his symptoms.
5. Antidepressants alone were insufficient because the underlying problem wasn't purely neurochemical—it was a substrate deficiency. You can't make dopamine and serotonin without adequate iron.
This is diagnostic psychiatry: systematic investigation of all possible causes, medical optimization first, and then—only if needed—psychiatric medication.
Conclusion: Medical Investigation Before Psychiatric Medication
If you're reading this and thinking, "This sounds like me," you're not alone. Low ferritin is one of the most common—and most overlooked—medical causes of psychiatric symptoms.
Here's what I want you to take away:
Your symptoms are real. Depression, anxiety, brain fog, and crushing fatigue are not "just in your head." They are the brain's way of signaling that something is wrong—and often, that something is correctable.
"Normal" labs aren't always normal. A CBC within reference range does not rule out iron deficiency. Ferritin must be specifically checked, and it must be interpreted in the context of optimal brain function—not just absence of anemia.
You deserve thorough investigation. Before accepting a psychiatric diagnosis and lifelong medication, you deserve a provider who will systematically investigate medical causes. After 19 years in the ICU, I can tell you this: the body always tells a story. Psychiatric symptoms are often the final chapter of an untold medical narrative.
Treatment works when diagnosis is accurate. When we identify and treat the underlying cause—whether it's low ferritin, thyroid dysfunction, vitamin deficiencies, or hormonal imbalances—symptoms often improve dramatically. Sometimes medications are still needed, but they work better when medical factors are optimized first.
Frequently Asked Questions
How much does a comprehensive assessment cost?
The initial 90-minute comprehensive medical-psychiatric assessment is $500. This includes:
Detailed symptom and medical history review
Physical examination when clinically indicated
Lab order review and interpretation
Personalized treatment plan
Written summary of findings and recommendations
Follow-up visits (30 minutes) are $200 and typically occur monthly during the optimization phase, then every 3 months for maintenance.
Lab costs vary depending on your insurance coverage and which panels are ordered. Most comprehensive panels (including ferritin, iron studies, thyroid, vitamins, metabolic panel, CBC) run $150-400 if paying out-of-pocket, but many insurance plans cover diagnostic labs with a copay.
Do you accept insurance?
Horizon Peak Health operates on a private-pay model for visits, meaning you pay for consultations directly at the time of service. However:
Lab Testing: Most insurance plans cover diagnostic lab work when medically necessary. I provide detailed lab orders that you can take to any in-network lab (Quest, LabCorp, hospital-based labs). Your insurance will process the labs according to your plan benefits.
Superbills: After each visit, I provide a detailed superbill (receipt) that you can submit to your insurance company for potential out-of-network reimbursement. Reimbursement rates vary by plan—some patients receive 50-80% back, others receive less or none. Check your out-of-network benefits to understand your coverage.
Prescriptions: If medications are prescribed, they're processed through your pharmacy insurance as usual.
This model allows me to spend 90 minutes on initial assessments and truly investigate your case systematically—something that's impossible in the 15-minute appointments typical of insurance-based practices.
How long does the process take?
Here's a realistic timeline:
Initial Assessment: 90 minutes (can be done via telehealth or in-person)
Lab Results: 3-7 days after blood draw
Follow-Up #1 (Results Review): 30 minutes, typically scheduled 1-2 weeks after labs
Review all findings
Finalize treatment plan
Start supplementation/medications if needed
Follow-Up #2 (Progress Check): 30 minutes, 4-6 weeks later
Assess symptom changes
Adjust treatments as needed
Address side effects
Lab Recheck: 8-12 weeks after starting treatment
Verify ferritin and other markers are improving
Adjust dosing if needed
Ongoing Care: Monthly visits during optimization (months 2-4), then every 3 months for maintenance
Most patients notice significant improvement within 2-3 months once we've identified and treated all contributing factors. Full optimization may take 4-6 months depending on severity of deficiencies.
What if you don't find anything wrong with my labs?
This is an important question—and the answer separates diagnostic psychiatry from standard practice.
If comprehensive lab testing shows no medical abnormalities, that's actually valuable information. It tells us:
1. Your symptoms aren't being driven by correctable nutritional or hormonal deficiencies—so we can focus psychiatric treatment more confidently
2. We may need to investigate further—some conditions require specialized testing (cortisol dysfunction, autoimmune markers, inflammatory panels, genetic testing for medication metabolism)
3. Psychiatric treatment may be the primary need—and that's okay. Sometimes depression, anxiety, or other conditions are primary psychiatric illnesses that respond well to evidence-based therapy and medication
The difference is that we've ruled out medical causes systematically rather than assumed everything is psychiatric from the start. This prevents years of ineffective treatment and ensures we're addressing the actual problem.
I don't view "no medical findings" as a failure—I view it as essential diagnostic clarity that allows us to treat more effectively.
What if I live outside California or Arizona?
Currently, I'm licensed to practice in California and Arizona, which means I can provide telehealth services to residents of these states. If you live elsewhere, I cannot provide direct clinical care.
However, you can:
Use the information in this article to advocate with your local providers
Seek a provider in your state who practices integrative psychiatry or functional medicine
Consider whether relocating care to a CA/AZ provider via telehealth is feasible if you have flexibility in residence
I'm working toward additional state licensures to expand access—follow Horizon Peak Health for updates.
When should I seek immediate care instead of booking a consultation?
Go to the emergency department or call 911 if you experience:
Active suicidal thoughts with a plan or intent to harm yourself
Thoughts of harming others
Severe confusion or disorientation
Hallucinations or delusions causing dangerous behavior
Chest pain, severe shortness of breath, or other medical emergencies
Severe panic attacks with loss of consciousness
Seek urgent psychiatric care (crisis line, urgent psychiatric clinic) if you have:
Worsening suicidal thoughts without immediate plan
Severe anxiety or panic that's unmanageable
Rapid mood changes or emotional instability that's dangerous
Medication side effects causing severe distress
Book a comprehensive assessment if you have:
Chronic, persistent symptoms (depression, anxiety, fatigue, brain fog) lasting weeks to months
Treatment-resistant symptoms despite trying medications
Symptoms that seem "medical" but haven't been fully investigated
Desire for thorough diagnostic workup before starting psychiatric medications
My practice focuses on comprehensive, systematic evaluation for chronic symptoms—not acute crisis intervention. If you're in crisis, please access emergency services first, then we can work together on long-term optimization once you're stable.
What If Iron Isn't My Problem?
I want to be clear: low ferritin is one common medical cause of psychiatric symptoms, but it's not the only one.
Diagnostic psychiatry means investigating all possible contributors systematically. Here are other medical factors I routinely evaluate:
Thyroid Dysfunction
Even "subclinical" hypothyroidism (TSH 2.5-4.5 mIU/L) can cause depression, fatigue, and cognitive slowing
Optimal TSH for symptom resolution: 1.0-2.5 mIU/L
Free T3 levels matter—some people convert T4 to T3 poorly
Vitamin Deficiencies
Vitamin B12: Essential for nerve function and mood regulation (target >600 pg/mL)
Vitamin D: Deficiency (<30 ng/mL) linked to depression and fatigue (target 50-70 ng/mL)
Folate: Required for neurotransmitter synthesis (especially important if taking antidepressants)
Magnesium: Deficiency causes anxiety, insomnia, muscle tension
Hormonal Imbalances
Testosterone (men): Low testosterone causes fatigue, depression, cognitive slowing
Estrogen/Progesterone (women): Perimenopause, PMDD, postpartum hormonal shifts
Cortisol: Chronic stress or adrenal dysfunction affects energy and mood regulation
Inflammation and Autoimmunity
Elevated CRP, chronic infections, autoimmune conditions drive psychiatric symptoms
Hashimoto's thyroiditis (autoimmune hypothyroidism) extremely common in treatment-resistant depression
Celiac disease, inflammatory bowel disease affect nutrient absorption
Sleep Disorders
Obstructive sleep apnea causes fatigue, brain fog, irritability, depression
Restless legs syndrome disrupts sleep architecture and causes secondary psychiatric symptoms
Metabolic Dysfunction
Insulin resistance and prediabetes cause energy crashes, brain fog, mood instability
Blood sugar dysregulation mimics anxiety and depression
During a comprehensive assessment, I investigate all of these factors—not just iron. The goal is to create a complete picture of what's driving your symptoms so we can treat effectively.
Iron deficiency is common and often overlooked, which is why this article focuses on it. But if your ferritin is optimal and you're still symptomatic, we keep investigating until we find answers.
What to Do Next
1. Request ferritin testing. Don't leave your doctor's office without a clear answer about whether ferritin will be checked. If they resist, advocate firmly or seek a second opinion.
2. Interpret your results critically. If your ferritin is below 75 ng/mL and you have psychiatric symptoms, don't accept "it's normal" as the final answer. Discuss whether optimization to 75-100 ng/mL might help.
3. Treat systematically. If low ferritin is identified, commit to consistent iron supplementation and monitoring. It takes months to restore iron stores—don't expect immediate results, but trust the process.
4. Consider comprehensive assessment. If you're experiencing treatment-resistant depression, anxiety, or fatigue, it may be time to see a provider who practices diagnostic psychiatry—someone who investigates medical causes systematically before attributing everything to psychiatric illness.
At Horizon Peak Health, I apply ICU-level diagnostic rigor to psychiatric care. That means comprehensive medical-psychiatric assessment, thorough lab investigation, and treatment plans that address root causes—not just symptoms. Most patients achieve significant improvement within 2-3 months once we identify and treat all contributing factors.
If you're tired of being told "your labs are normal" when you feel terrible, I can help. Book a consultation to discuss whether comprehensive assessment is right for you. Let's investigate systematically, optimize thoroughly, and find out why you're not feeling your best.
Because you deserve answers—not just prescriptions.
---
References
- Beard, J.L., Connor, J.R. (2003). Iron status and neural functioning. Annual Review of Nutrition, 23, 41-58. PMID: 12704220
- Lozoff, B., Georgieff, M.K. (2006). Iron deficiency and brain development. Seminars in Pediatric Neurology, 13(3), 158-165. PMID: 17101454
- Shariatpanaahi, M.V., Shariatpanaahi, Z.V., Moshtaaghi, M., et al. (2007). The relationship between depression and serum ferritin level. European Journal of Clinical Nutrition, 61(4), 532-535. PMID: 17063146
- Patterson, A.J., Brown, W.J., Roberts, D.C. (2001). Dietary and supplement treatment of iron deficiency results in improvements in general health and fatigue in Australian women of childbearing age. Journal of the American College of Nutrition, 20(4), 337-342. PMID: 11506063
- Stahl, S.M. (2021). Stahl's Essential Psychopharmacology: Neuroscientific Basis and Practical Applications (5th ed.). Cambridge University Press.
---
Disclaimer: This article is for educational purposes only and does not constitute medical advice. Iron supplementation should be undertaken under medical supervision. High ferritin levels can indicate serious conditions including hemochromatosis and chronic inflammation. Always consult with a qualified healthcare provider before starting any supplementation regimen or making changes to your treatment plan.
---
About the Author:
Canybec Sulayman, PMHNP-BC, brings 19 years of ICU nursing experience across seven specialties to psychiatric care at Horizon Peak Health. He specializes in diagnostic psychiatry—systematic investigation of medical and psychiatric causes of symptoms—using comprehensive assessment and evidence-based treatment. Board-certified in psychiatric-mental health nursing, Canybec serves patients in Los Angeles, Phoenix, and via telehealth throughout California and Arizona.
Horizon Peak Health
Los Angeles & Phoenix | Telehealth Available
Book a consultation: horizonpeakhealth.com/contact
Canybec Sulayman, PMHNP-BC
Diagnostic Psychiatry Specialist
Investigating the root causes of mental health symptoms with 19 years of ICU diagnostic rigor.